Disclaimer: These videos are to be used as a reference tool to the suicide care pathway. They provide an overview but are not comprehensive of the entire pathway.
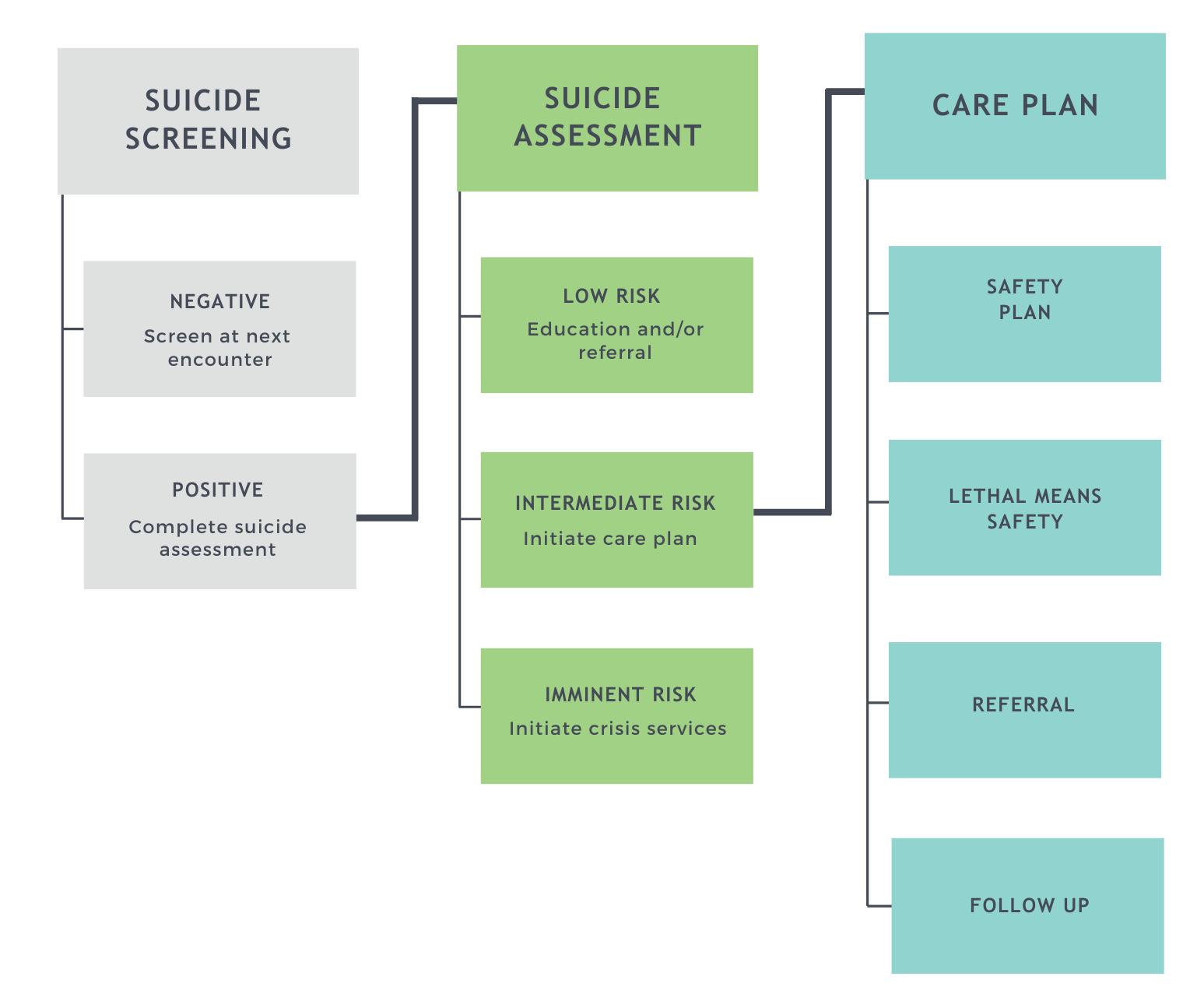
Suicide Screening
All patients ages 12-24 should complete the Ask Suicide-Screening Questions (asQ) screening tool at every provider visit or the frequency determined by your clinic. Targeted screening is recommended for patients ages 8-11 who are at higher risk for thoughts of suicide. The screen can be given by paper or verbally by staff. If given verbally, screening should be direct, non-judgmental, and verbatim to the screener. Here is an example of a staff member performing verbal screening:
After Video Survey:
After watching the video, please take this Screening Survey.
Complete the asQ BSSA for all patients who screen positive or have numerous warning signs and risk factors of suicide. The asQ BSSA is a brief risk assessment tool that assesses risk factors, protective factors, and warning signs. It focuses on determining current suicidal thoughts, past suicidal behavior, comorbid symptoms, and the presence of social supports and stressors.
Here is a video example of a staff member completing a BSSA with a patient at risk for suicide:
After Video Survey:
After watching the video, please take this Assessment Survey.
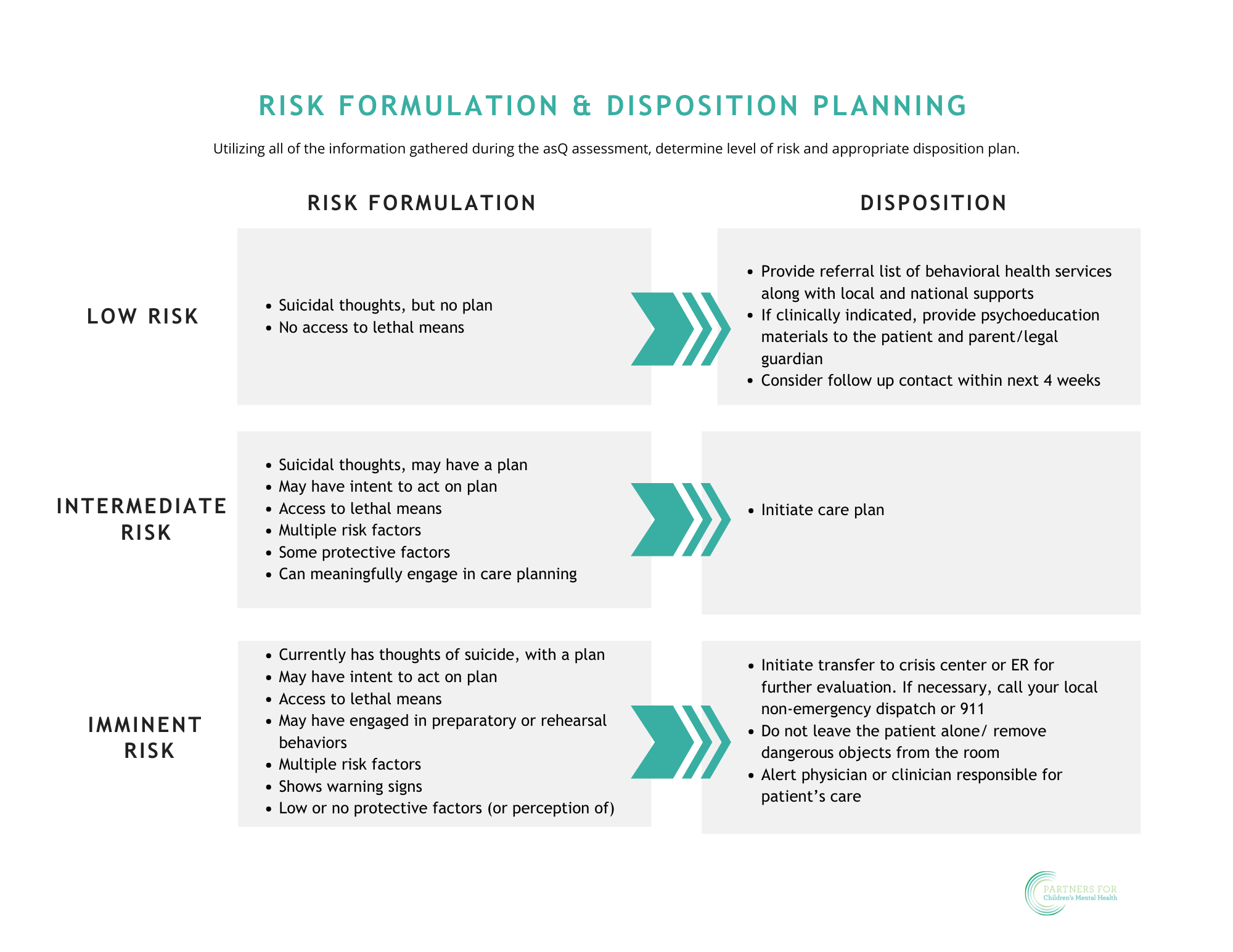
If the risk level on the BSSA is:
Low Risk
- Provide referral list of behavioral health providers along with local and national resources.
- If clinically indicated, provide educational materials to the patient and parent/legal guardian.
- Consider follow up contact within next 4 weeks.
Intermediate Risk
Initiate care plan using least restrictive level of care.
Imminent Risk
Initiate immediate transfer to crisis center or ER for further evaluation.

Safety Plan
- Recommended tool: Stanley Brown Safety Plan.
- Collaboratively develop a safety plan with the patient and review with parent/legal guardian the same day that suicide risk is identified.
- Provide educational materials to the patient and family regarding symptoms and when to utilize safety plan.
Safety plans are most powerful when developed collaboratively with a provider or parent. Here is an example of engaging a patient in completing a safety plan:
After Video Survey:
After watching the video, please take this Safety Planning Survey.
Means Safety
- Discuss means safety and provide educational materials to patient and parent/legal guardian the same day risk is identified.
- Ensure the parent/legal guardian has a plan to secure lethal means including firearms, medications, drugs, knifes, etc.
Lethal means safety conversations should come from a place of seeking to understand and focusing on safety. Voluntary removal or safe storage of firearms, medications, and dangerous sharps has been shown to save lives:
After Video Survey:
After watching the video, please take this Lethal Means Safety Counseling Survey.
Referral to behavioral health care
- If behavioral health provider is integrated, refer the patient and parent/legal guardian within your practice.
- Otherwise, refer the patient and parent/legal guardian to behavioral health providers or systems that provide evidenced-based care specific to suicide risk.
- Create and annually update a community specific resource/referral list of behavioral health providers.
Follow up
- 48 hours after visit, conduct a telephone outreach to check in regarding:
- Assessment of current suicide risk
- Engagement in recommended behavioral health care
- Utilization of safety plan
- Means safety follow up
Follow-up can occur by phone or in person. It does not have to be long but should hit the high points above:
After Video Survey:
After watching the video, please take this Referral Survey.