Better support young patients at risk for suicide
Written by Dr. Brian Pitts, MD, FAAP, Provider Consultant at PCMH
Supporting youth experiencing suicidal thoughts can feel daunting. In my early career, patients with thoughts of suicide terrified me. I wasn’t sure exactly what to ask or how to ask it and had minimal confidence about what I could do to help keep patients safe. I was afraid to miss something or make a mistake. I wasn’t sure how to care for these patients while balancing the rest of my caseload. It took learning, practice, and feedback for me to turn the corner and make suicide prevention and intervention a clinical strength.
Now, I leverage that expertise in my role as a provider consultant with Partners for Children’s Mental Health(PCMH). PCMH is a community-facing center established by Children’s Hospital Colorado and the University of Colorado School of Medicine to improve youth mental health in Colorado.
At PCMH, we created the Pathway to Suicide Prevention (PSP) program to help providers deliver suicide-safer care. Through PSP, PCMH offers free training and consultation to help clinics implement a youth suicide prevention care pathway rooted in the Zero Suicide framework. The care pathway includes screening, risk assessment, safety planning, lethal means safety, and follow-up. It features evidence-informed suicide prevention practices backed by the American Academy of Pediatrics, the American Foundation for Suicide Prevention, and the National Institutes of Mental Health. Providers learn what to do when a patient expresses thoughts of suicide and how to keep them safe until they receive the right support.
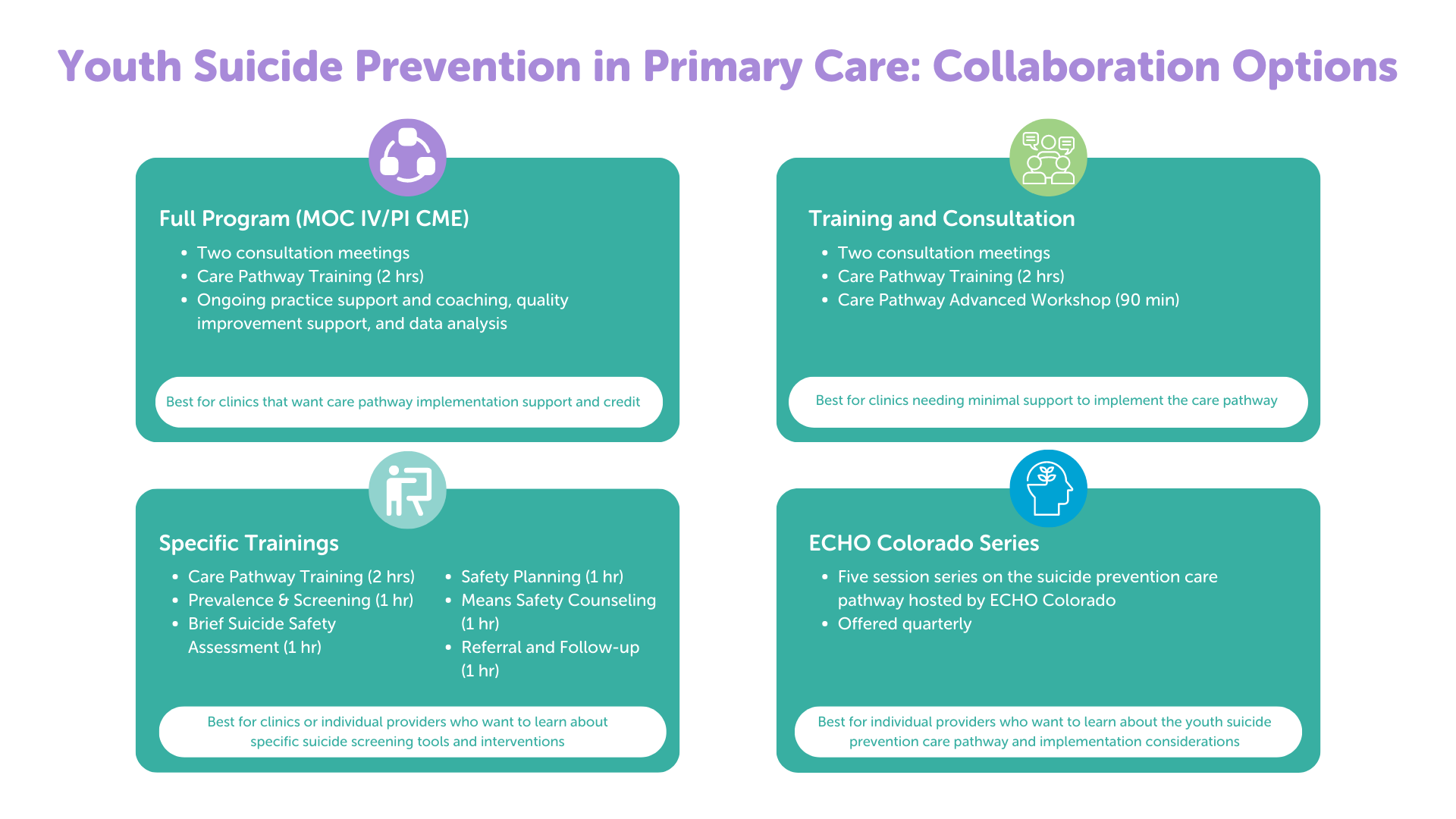
Depending on individual clinic needs, participating clinics can receive:
- Two one-hour trainings on the care pathway
- Two consultation meetings
- Ongoing practice support and coaching, quality improvement support and data analysis
- MOC4 (pediatricians) or PI-MOC/CME (FP/NP/PA) for participants
Since launching the program in 2020 we’ve seen strong results across clinics. Participating practices are now screening for suicide at 80% of all teen well visits. On average, 9% of teens screened require further assessment. By taking an extra 20-30 seconds per well visit, partner clinics have detected more than 200 youth experiencing thoughts of suicide.
This year, we’re recruiting new Colorado clinics to join our program. Don’t miss this opportunity to take your clinic to the next level.
If you are interested in getting involved or have questions, please email info@pcmh.org. If you know clinics that would benefit from the program, please share the program flyer or this video.
Dr. Brian Pitts is an emerging adolescent medicine specialist and primary care physician. He served on the advisory group in the development of the AAP Blueprint on Suicide Prevention. Note: This post originally appeared in the AAP-CO newsletter.